Dental implants have become the preferred way to replace missing teeth owing to their superior longevity and durability. Unlike dental bridges, which have an average lifespan of 10-15 years, dental implants are designed to last a lifetime and have an exceptionally high success rate. Research demonstrates that dental implants have a lifespan of up to 50 years and succeed in approximately 95-98% of cases.
Nonetheless, if you plan to have dental implant surgery, it is vital to understand the factors and conditions that can cause dental implants to fail prematurely. The type of dental implant you have, your health status, and the density of your jawbone, for example, can all influence the success rate of dental implants. Correct post-surgical care is also crucial to ensure dental implants heal without complications.
In the following guide, we will explore the causes and signs of premature dental implant failure and discuss potential treatments:
Table Of Contents
What is Dental Implant Failure?
Dental implant failure occurs when a dental implant does not successfully integrate with the surrounding bone tissue or experiences complications, such as infection, that prevent it from functioning as intended. Dental implant failure can occur within the first few months after placement (early implant failure) or many years later (late implant failure). In some cases, dental implant failure is reversible with treatment; in other cases, however, removing or replacing the implant is necessary to protect the patient’s health or correct issues with improper positioning.
Common Causes of Dental Implant Failure
The complexity of dental implant surgery varies considerably depending on where the implants are placed and the patient’s bone density. Implants placed in the maxilla (upper jawbone), for example, may require preliminary sinus lift surgery and generally have a higher risk of complications than implants placed in the mandible (lower jaw). Other factors that can lead to premature dental implant failure include:
Poor Osseointegration: Osseointegration is the process by which the implant fuses with the jawbone. If this process is disrupted due to factors like inadequate bone quality or quantity, infection, or excessive force placed on the implant during healing, it can lead to implant failure.
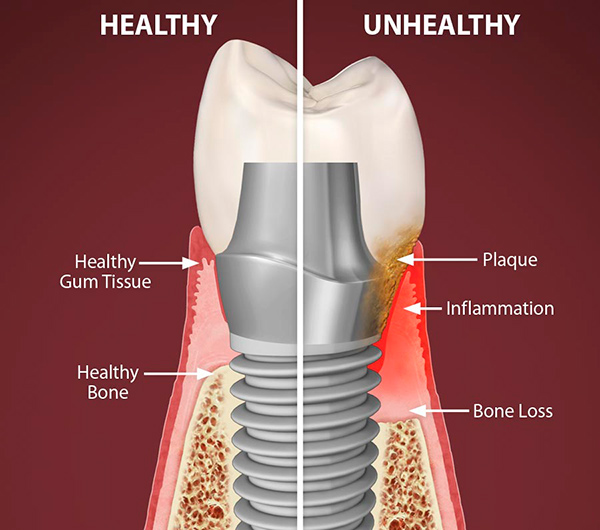
Infection: Though significant post-surgical infections are rare after dental implant placement, some patients can develop peri-implantitis months or even years after getting dental implants. Peri-implantitis is a condition similar to gum disease that affects the tissues around the implant, causing inflammation and gum recession. If left untreated, it can also cause bone loss and ultimately lead to implant failure.
Poor Oral Hygiene: Inadequate oral hygiene can result in the buildup of plaque and bacteria around the implant, increasing the risk of peri-implantitis and decay in surrounding teeth, which play a role in supporting the implant. Proper home care using dentist-recommended products and regular dental cleanings are essential for implant longevity.
Medical Conditions: Certain systemic conditions such as diabetes, autoimmune disorders, and osteoporosis can affect the body’s ability to heal and integrate with the implant, increasing the risk of failure. By impairing the normal function of the blood vessels and immune system, these health issues also put patients at risk of late dental implant failure. Likewise, the use of medications that cause dry mouth may increase the risk of peri-implantitis, as can lifestyle factors like tobacco use. Tobacco use reduces blood flow, delays healing, and increases the risk of infection, all of which can compromise the success of dental implants.
Mechanical Issues: Chronic grinding or clenching of teeth (a condition known as bruxism) can exert excessive pressure on the implant and surrounding bone, leading to implant failure over time. If you suffer from bruxism, your dentist may recommend a night guard or occlusal adjustment to protect the implant.
Allergic Reactions: Because dental implants consist of biocompatible materials, allergic reactions following surgery are exceedingly rare – but they can happen, especially in people with allergies to metals. If you’re concerned about allergic reactions, consider having yourself screened for an allergy to titanium prior to surgery.
To prevent dental implant failure, strictly adhere to your dentist’s aftercare instructions while your implants heal. Avoid the use of tobacco products for at least three months after dental implant surgery, and stick to a soft food diet for two weeks (or as long as your dentist recommends). Practice good oral hygiene and attend regular follow-up appointments to ensure your implants have fused with the jawbone.
Recognizing the Signs of Implant Failure
After your dental implants have integrated with your jawbone, they should look and feel exactly like your natural teeth. As such, any discomfort or change in the position or stability of your implants should be cause for concern. Some signs that your implants may be at risk of failure include:
1. Persistent Pain or Discomfort: While some tenderness is to be expected in the weeks immediately following dental implant surgery, chronic discomfort should never be ignored. Persistent or increasing pain or swelling around the implant site can be a sign of poor osseointegration, infection, or other complications.
2. Bleeding or Discharge. Bleeding around the dental implant that occurs more than two weeks after surgery, especially during brushing or flossing, can be a symptom of gum inflammation or peri-implantitis. The presence of pus anywhere around the implant site (at any stage of healing) is a sign of infection and requires immediate attention from a dental professional.
3. Loose or Shifting Implants: If a dental implant feels loose or unstable, it may be a sign of poor integration with the surrounding bone or mechanical complications resulting from excessive bite force or bruxism. Similarly, if you experience changes in your bite alignment, discomfort when biting or chewing, or a feeling of the implant being out of place, it may indicate potential failure. Implant shifting can occur many years after placement due to natural changes in the shape of the jawbone and the position of the surrounding teeth, which is one reason why regular monitoring from a dentist is essential to maintain dental implants.
4. Gum Recession: Receding gums around the dental implant can expose the implant abutment or post, leading to aesthetic concerns and potential implant failure. When the gum tissue around the implant recedes, it creates spaces where food particles and bacteria can become trapped, significantly increasing the risk of peri-implantitis, inflammation, and other oral health complications.

5. Metallic Taste or Bad Breath: Persistent bad breath or a metallic taste in the mouth may indicate infection or gum recession around the implant. Bad breath is also a common sign of gum disease and tooth decay, so it should always be assessed by a dental professional.
If you experience any of these symptoms, schedule an appointment with your dentist as soon as possible – even if they seem mild. In many cases, prompt diagnosis and treatment can prevent dental implant failure.
Diagnosis and Treatment Options
Diagnosing and treating dental implant failure requires a comprehensive evaluation by a dental professional to identify the underlying cause and develop an appropriate treatment plan. Your dentist will begin by conducting a thorough clinical examination to assess the implant site, checking for signs of inflammation, infection, mobility, or other abnormalities. During the exam, X-rays, CT scans, or other imaging studies may be used to evaluate the viability of the implant, surrounding bone, and soft tissues. You will also be asked to describe your specific symptoms, such as the location and intensity of the discomfort, to help determine the potential cause of implant failure, along with any changes in your oral health history, lifestyle, or medications.
Your dentist will then evaluate the level of osseointegration between the implant and the surrounding bone to determine if there are any issues with stability or integration. A mobility test may be performed to assess implant stability, and if peri-implantitis is suspected, a microbial analysis may also be conducted to identify the strains of bacteria present and select the correct antibiotic treatment.
Based on the results of these tests, a personalized treatment plan will be developed to address the specific cause of implant failure. Treatment options may include:
Non-Surgical Interventions: Mild cases of peri-implantitis or soft tissue infection may be managed with a combination of professional dental cleanings, antimicrobial rinses, and improved oral hygiene practices. Antibiotics may also be prescribed to eliminate infection below the gum line and prevent further complications.
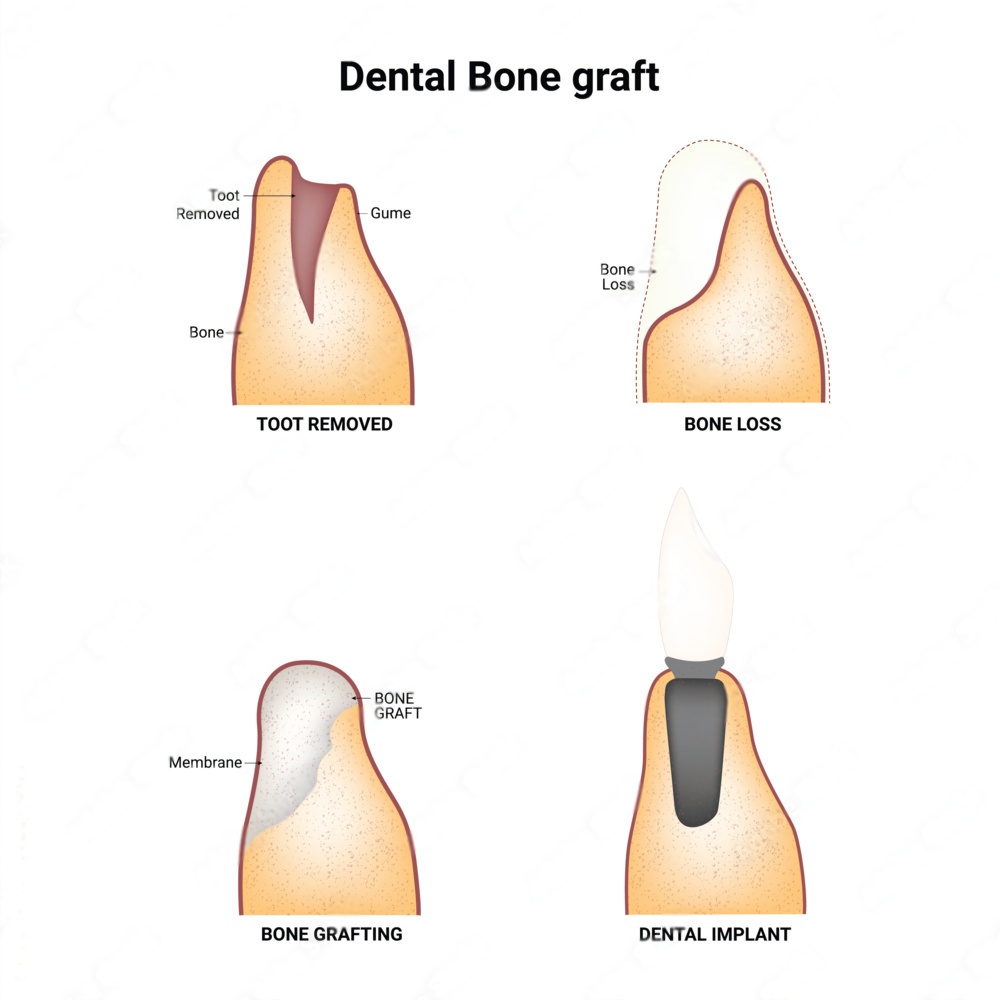
Surgical Interventions: Many dental implant complications can be resolved with minor surgical procedures, such as implant position adjustment, gum grafting, or the replacement of specific parts of the implant, such as the abutment or crown. However, advanced cases of peri-implantitis, bone loss, or mechanical issues may require more invasive surgical treatments, such as bone grafting, guided bone regeneration, implant removal, or replacement. Guided bone regeneration is an innovative treatment wherein a protective collagen membrane and a bioactive material are used to protect the implant site and stimulate bone growth, creating a more suitable foundation for the dental implant.
After treatment, regular follow-up appointments are essential to monitor healing, assess implant stability, and prevent the recurrence of complications. Enhanced oral hygiene practices, lifestyle modifications, and maintenance routines may also be recommended to support implant success.
Contact Dr. Dalmao For Any Concerns About Your Dental Implants
While dental implant failure is relatively uncommon, it is essential to work with a skilled and experienced dental professional who can effectively assess your oral health, identify potential risks, and develop a personalized treatment plan to maximize the success of your dental implant procedure. Many cases of dental implant failure can be prevented by treating underlying issues, such as gum disease, malocclusion, or poor bone density, before surgery. Likewise, regular follow-up appointments, diligent oral hygiene, appropriate surgical aftercare, and lifestyle modifications can help reduce the risk of implant failure and promote long-term implant stability and function.
As one of Mississauga’s leading oral surgeons, Dr. Oscar Dalmao can guide you through the dental implant process from start to finish, ensuring aesthetically pleasing, long-lasting results. In addition to performing routine dental implant surgery, Dr. Dalmao specializes in advanced and complex procedures, including bone grafting, tissue regeneration, and maxillary dental implant placement. Whether you are missing a single tooth or living with edentulism, our experts can help you choose the best dental implant plan to suit your needs, lifestyle, and budget.
Contact us today to discover how dental implants can restore your smile – and confidence.


