Table of Contents
What Problems Can an Uneven Bite Cause?

Multiple factors can contribute to gum recession, including:
Poor Oral Hygiene: Inadequate brushing and flossing can lead to plaque build-up, which can cause gum inflammation and recession over time. A lack of dental care also frequently leads to receding gums, as professional teeth cleaning is necessary to remove plaque from below the gum line and prevent gum disease.
Aggressive Brushing: Brushing too hard (or using a hard-bristled toothbrush) can damage the delicate gum tissue and contribute to gum recession.
Gum Disease: Periodontal diseases, such as gingivitis and periodontitis, frequently cause your gums to recede. As periodontal disease worsens, bacteria gradually destroy the gum tissue and supporting structures, exposing the root surfaces of the teeth and creating large pockets of missing gum tissue.
Lifestyle Factors: Smoking or chewing tobacco can contribute to gum recession by interfering with blood flow to the gums, causing inflammation, and reducing saliva production, all of which damage the gums and inhibit tissue repair. Many medications, including over-the-counter antihistamines, antacids, and pain relievers, can also increase the risk of gum recession, typically by impairing saliva flow. Inadequate saliva flow (a condition known as “dry mouth”) allows bacteria in the oral cavity to thrive and makes the teeth and gums more susceptible to acid erosion.
Aging and Genetics: Certain individuals may be more predisposed to gum recession due to genetic factors affecting the thickness and strength of their gum tissue. Similarly, though receding gums are not an inevitable part of getting older, many people experience a loss of gum tissue as they age. Age-related health conditions, including heart disease and diabetes, can predispose people to gum disease, as can hormonal changes, such as menopause. Older adults are also more likely to experience dry mouth and have a slower rate of tissue repair. According to one study, the percentage of adults with receding gums increases from 38% to 71% between the ages of 30-59. By age 80, 90% of people have some degree of gum recession.
Trauma or Injury: Trauma or injury to the gums can cause them to recede in the affected area. Gum recession is particularly likely to occur following a significant injury to the mouth or face wherein one or more teeth become loose. Certain facial piercings, such as lip piercings, can also cause gum recession by rubbing against the gums, which gradually wears them down.
Recognizing the Symptoms of Receding Gums
Though receding gums often cause tooth pain and sensitivity, this isn’t always the case; in fact, many people are unaware they have gum disease. Though only a dentist can accurately diagnose gum recession and other oral health problems, the following signs and symptoms may indicate that your gums are receding:
Longer-Looking Teeth: One of the earliest and most noticeable signs of gum recession is when your teeth appear longer than before. As the gums pull back, away from your teeth, you may see more of the tooth’s root surface, which is typically darker and more sensitive than the enamel-covered portion of the tooth.
Tooth Sensitivity: Increased sensitivity to hot, cold, or sweet foods and beverages can occur as the tooth roots become exposed. Even if you don’t have cavities, tooth roots are naturally sensitive to external stimuli because they aren’t protected by dental enamel, the hard outer coating that covers the chewing surfaces of the teeth.
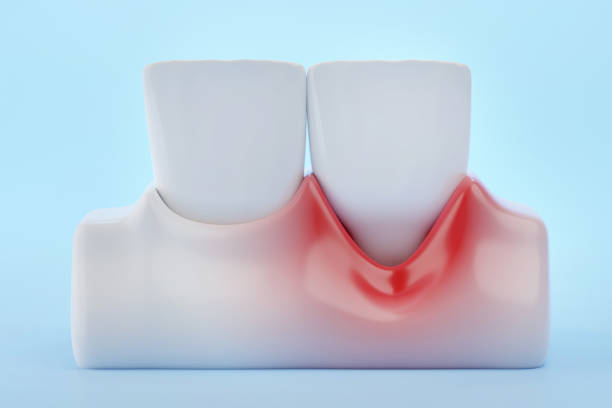
Gum Inflammation or Discolouration: Gums affected by recession may appear darker or redder than surrounding healthy gum tissue, particularly if gingivitis or periodontitis are present. You may also notice you have swollen gums (which can feel hot or tender) and bleeding, especially during brushing or flossing.
Gumline Changes: An irregular or uneven gumline can result from the gum tissue receding in specific areas, creating a scalloped or notched appearance along the teeth. Cosmetic dental procedures, such as gum contouring, are often used to correct this issue and create a more even gum line.
Bad Breath: Persistent bad breath or a bad taste in the mouth may result from bacteria accumulating in the gaps between the teeth and receding gums. Bad breath may also indicate the presence of periodontal disease.
Loose or Shifting Teeth: As gum recession progresses, it can lead to changes in the position or stability of the teeth, causing them to feel loose or shift. Problems with bite alignment occur because gum recession eventually damages the deeper tissues, ligaments and bone that hold your teeth in place, eroding their foundation.

Pain or Discomfort: Discomfort, pain, or tenderness in the gums or teeth, especially when chewing or applying pressure, can indicate advanced gum recession and potential damage to the underlying structures. However, there are many potential causes of dental pain, so it’s essential to see your dentist to rule out more serious issues, such as an infected or cracked tooth.
If you notice any of these symptoms, schedule a dental exam as soon as possible. Early intervention and proper dental care can help prevent further gum recession, address underlying issues, and maintain optimal oral health. Treating gum disease in its early stages will also prevent more severe problems from developing, such as infection and tooth loss.
Potential Complications
Left untreated, receding gums can predispose people to developing multiple oral health concerns, such as:
Tooth Decay: Because the roots of the teeth lack protection from dental enamel, they are highly susceptible to developing decay and cavities when exposed due to gum recession. Cavities that develop in the roots of the teeth are particularly dangerous (and painful); once a hole forms in the root of a tooth, the pulp inside it can quickly become inflamed and infected, requiring root canal surgery.
Gum Disease: Receding gums often create pockets or gaps between the teeth and gums that trap food particles and provide a breeding ground for disease-causing bacteria. These pockets are often very difficult to clean with routine brushing and flossing, so they can increase the risk of gingivitis and periodontitis even in people who practice good oral hygiene.
Tooth and Bone Loss: Advanced periodontal disease can cause infection in the jawbone and compromise the supporting structures of the teeth, causing bone resorption and changes in bite alignment (malocclusion). Malocclusion places additional stress on the teeth and gums, makes it more difficult to speak and chew properly, and may contribute to painful jaw joint issues. Eventually, the combination of increased wear and weakening bone and ligaments that accompany gum recession can cause affected teeth to become loose and fall out.
For older adults, this can be the beginning of a dangerous cycle: Having missing teeth increases problems with bite alignment and leads to further bone loss, negatively impacting the health of surrounding teeth. Unless the underlying gum disease is treated and missing teeth are restored (using dental implants or bridges), the patient will continue to have an elevated risk of further tooth loss.
Systemic Health Risks: Periodontal disease has been linked to multiple systemic health issues, such as cardiovascular disease, diabetes, respiratory infections, and chronic inflammation. Treating gum recession (and other forms of gum disease) is therefore an essential part of healthy aging.
Management and Treatment Options
In most cases, treating gum disease is simple, painless, and very affordable. Modern advances in dental technology and techniques allow dentists to repair and protect damaged gums using minimally invasive procedures that produce rapid, aesthetically pleasing results. Some of the most common treatments for gum disease include:
Lifestyle Changes: In some cases, improving oral hygiene or making lifestyle modifications may be all that is required to treat receding gums. Your dentist may recommend more frequent dental cleanings, the use of specific products to care for your teeth (for example, a water flosser to clean gum pockets, a soft-bristled toothbrush, or sensitivity toothpaste to reduce discomfort), or smoking cessation (if you smoke). Other helpful lifestyle interventions may include increasing saliva flow by drinking more water or chewing sugar-free gum and eating a more nutritious, anti-inflammatory diet.

Scaling and Root Planing: Scaling and root planing are specialized deep-cleaning procedures that remove plaque and tartar below the gum line. Root planing also smooths the root surfaces of affected teeth, making it easier for gum tissue to heal over them and form a strong attachment.
Gum Grafting: In this surgical procedure, tissue from another part of the mouth (such as the palate) or a donor source is used to cover the exposed tooth roots and restore gum tissue volume. Gum grafting is typically only required for advanced cases of gum disease that have not responded to other types of treatment.
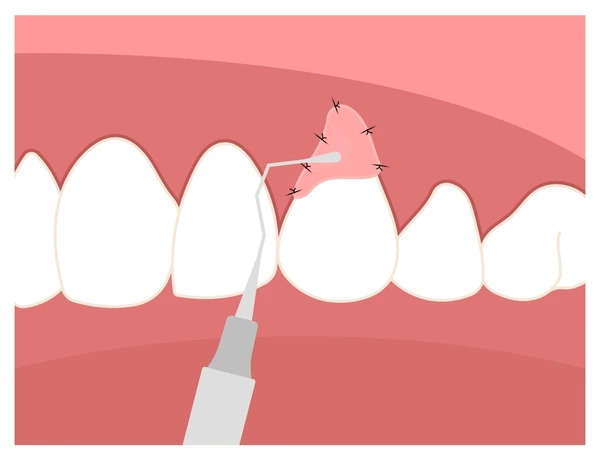
Pinhole Surgical Technique (PST): PST is a minimally invasive procedure that involves making small holes in the gum tissue and repositioning it with specialized dental instruments. PST can cover exposed tooth roots without gum grafting, making it an attractive alternative for patients with advanced gum recession. PST has a rapid recovery time and does not cause significant post-surgical discomfort, bleeding, or inflammation. It also does not require the use of sutures.
How to Prevent Gum Recession
Gum recession is usually preventable using good oral hygiene practices, healthy lifestyle habits, and by avoiding injury to the teeth and gums. The following strategies can help people of all ages ward off receding gums:
1. Practice gentle but thorough oral hygiene.
Use a soft-bristled toothbrush and gentle, circular motions to brush your teeth twice daily. Avoid brushing too hard or using a hard-bristled brush, as this can damage the gums and enamel. Clean between your teeth at least once daily with dental floss or interdental brushes to remove plaque and food debris, then finish by rinsing with an antimicrobial mouthwash. Excellent home care is one of the best ways to reduce the build up of plaque and bacteria that can lead to gum inflammation and recession.
2. See your dentist for regular check-ups.
Visit your dentist for a check-up and professional teeth cleaning at least twice a year. During routine dental exams, your dentist will look for early signs of tooth decay and gum disease and remove plaque from below the gum line, helping to prevent gum recession. If you’re older or at high risk for gum disease, your dentist may recommend more frequent dental cleanings, enhanced oral hygiene at home, or lifestyle modifications to protect against gum disease, helping you avoid the need for more invasive procedures later on.
3. If you smoke, quit.
Quitting smoking (and avoiding the use of other tobacco products) is one of the most effective ways to prevent gum disease and improve your overall health. If you are struggling to quit smoking, talk to your dentist or doctor about smoking cessation aids, such as nicotine patches, to help you manage cravings while healing your gums.
4. Protect your teeth and gums from injury.
Wear a custom-fitted mouth guard when playing high-impact sports and avoid getting piercings that may rub against the gums, such as lip piercings. Do not chew on pens, ice, or other hard objects.
Conclusion
Though gum recession may seem like a normal part of aging, it should never be ignored. Ensuring your tooth roots remain covered by a healthy layer of gum tissue is crucial to prevent the development of tooth decay, periodontitis, bite misalignment, tooth loss, and other oral health concerns. Pink, symmetrical gums also make your smile look brighter and more youthful, offering noticeable cosmetic benefits.
If you think you may have receding gums, our skilled team of dental professionals can help. As one of Mississauga’s leading periodontists, Dr. Oscar Dalmao offers multiple advanced and minimally invasive treatment options for gum disease and recession, making it possible to restore your smile without discomfort. Contact us today to learn more about your options for preventing and reversing gum disease and recession.


