If you have missing teeth, dental implants can rejuvenate your smile, preserve your facial shape, and maintain the health of your jawbone. In some cases, however, patients who have experienced substantial bone loss due to missing teeth or gum disease require bone grafting before dental implant placement. Bone grafting uses transplanted bone to restore the jawbone, replacing lost volume so the jaw can adequately support dental implants or other restorations. By investing in bone grafting, patients can ensure the structural integrity of their dental implants and enjoy the confidence and functionality of a fully restored smile for many years to come.

What is Bone Grafting & How is It Used in Dentistry?
Bone grafting is a surgical procedure that involves the placement of natural or synthetic bone material into areas of the jaw that have experienced significant bone loss or deterioration, often as a result of tooth extraction, periodontal disease, or other dental issues. Bone grafting plays a vital role in restoring and maintaining the health and structure of the jawbone, creating a solid foundation for dental implants and certain periodontal treatments.
Bone grafts are used in dentistry is to stimulate the body’s natural bone regeneration process, providing a solid foundation for dental implants (or other restorative procedures). By rebuilding and strengthening the jawbone, bone grafting ensures the long-term success and stability of dental implants, dentures, or other prosthetic devices.
Why It’s Necessary
Following tooth extraction or loss, the bone surrounding the supporting structures of the tooth may deteriorate over time due to lack of stimulation from the tooth root. Periodontal disease, congenital defects, certain medical conditions, and trauma to the jawbone can also lead to bone loss.
Because dental implants are attached to titanium or ceramic posts anchored in the jawbone, any reduction in jawbone density can impede the long-term viability of implants. As such, dentists typically recommend having dental implants placed within six months of tooth loss or extraction to prevent the need for bone grafting. However, in instances where this is not possible, bone grafting procedures can restore lost bone structure (or preserve existing structure) by promoting new bone growth and preventing bone resorption, which is essential for maintaining oral health and supporting future dental treatments.

Types of Bone Grafts for Dontal Implants
In dentistry, several types of bone grafts can be used to regenerate bone in the jaw in preparation for dental implant placement, periodontal treatment, and other dental procedures. Some of the most common types of bone grafts used in dentistry include:
1. Autografts
Autografts (or autogenous bone grafts) involve using healthy bone from the patient’s own body, typically from a donor site within the patient’s hip (though tissue from the tibia may also be used). Autografts are considered the gold standard for bone grafting due to their high success rate and compatibility with the patient’s body, reducing the risk of rejection or complications. The only drawbacks of autografts are potential discomfort at the site where tissue is removed and limitations on the amount of tissue that can be harvested. However, because dental implants and periodontal treatments are minimally invasive, autografts are usually sufficient for dental procedures.
2. Allografts
Allografts consist of human donor bone obtained from tissue banks. Allograft bone is sterilized, processed, and stored for surgical use. When implanted, it provides a scaffold for new bone growth and is gradually replaced by the patient’s natural bone structure over time.
Allografts may be preferred by some patients because they eliminate the need for a second surgical site (to collect bone tissue from the patient). However, they carry a slightly higher risk of infection and rejection and may be less robust than autografts.
3. Xenografts
Xenografts utilize bone graft materials derived from animal sources, typically bovine (cow) or porcine (pig) bone. Xenograft materials are processed to remove organic components and impurities, leaving behind a sterile mineral scaffold that promotes new bone formation. Xenografts are biocompatible and can stimulate the body’s natural bone regeneration process, but they carry a higher risk of rejection and poor osseointegration than other types of bone graft.
4. Alloplastic/ Synthetic Bone Grafts
Alloplastic grafts contain synthetic bone substitutes made from biocompatible materials such as calcium phosphate, hydroxyapatite, or bioactive glass. These materials mimic the mineral composition of natural bone and provide a scaffold for new bone growth. Hydroxyapatite is the most popular choice for alloplastic grafts due to its strength, durability, and superior biocompatibility. Because human bone already contains a significant amount of hydroxyapatite, this material readily integrates with the jawbone.
Alloplastic grafts offer versatility, predictable resorption rates, and lack the need for a living donor, making them a convenient choice for dental bone grafts.
Each type of bone graft material has unique characteristics, advantages, and cost considerations. As such, you should choose a knowledgeable oral surgeon to perform this procedure and discuss your concerns and treatment goals thoroughly during the consultation. Your oral surgeon can then customize your bone grafting procedure to ensure optimal results.
Understanding the Bone Grafting Procedure
During the initial consultation with your dentist or oral surgeon, you can expect to discuss your dental health, review your medical history, and explore different treatment options. Your dentist will then use imaging tests (such as X-rays and CBCT scans) to evaluate the amount of bone loss in your jaw and determine the need for bone grafting. If you are a good candidate for this procedure, your dentist will help you select the best bone grafting material to meet your needs, plan your procedure, and provide aftercare instructions.
On the day of the procedure, you will receive local anesthesia and sedation to ensure comfort during the bone grafting surgery. (General anesthesia may be used for more complex cases or patients with dental anxiety, but most bone grafts can be completed using only local anesthesia.) Then, the dentist will create a tiny incision in your gum tissue before placing the graft material where bone regeneration is needed. During healing, the graft material will serve as a scaffold that stimulates new bone growth while integrating with the existing bone.
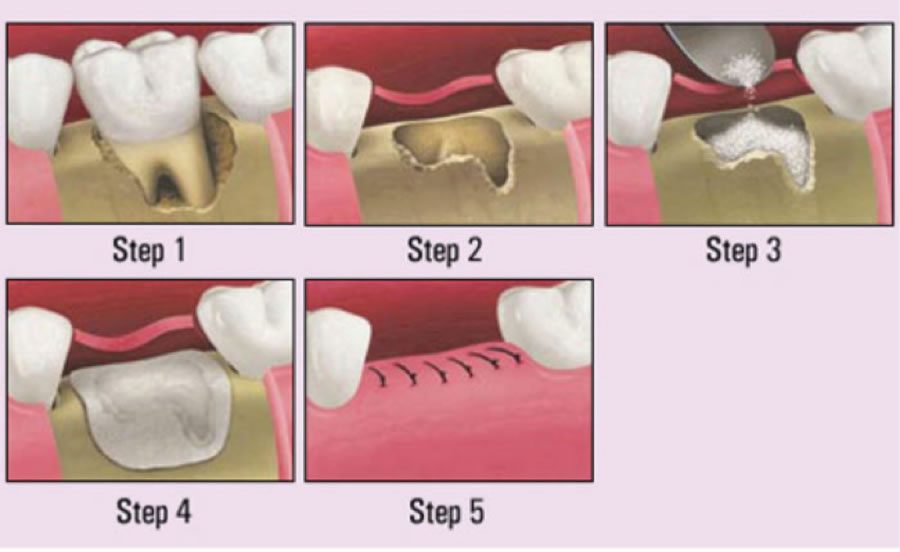
Once the graft material is placed, the incision is sutured closed, and the surgical site is covered with a protective membrane or barrier to facilitate healing and prevent infection. The body’s natural healing process will gradually replace the graft material with new bone tissue over several months. (Note that individual healing times may vary depending on the type of graft received and the patient’s health status.) During the healing period, your dental surgeon will schedule regular follow-up appointments to assess the amount of bone regeneration. Based on their observations, they will let you know when you can safely have dental implants placed.
Benefits of Bone Grafting
For those who have suffered a loss of jawbone density due to tooth loss or other factors, bone grafting has multiple advantages, such as:
1. Improved stability and longevity of dental implants.
Adequate bone volume and density are essential for ensuring the stability and long-term success of dental implants. Bone grafting creates a strong foundation for the implant post to be securely anchored within the jawbone, allowing it to withstand the forces exerted by chewing, speaking, and other daily activities.

In patients with insufficient jawbone density, the implant post may fail to integrate properly with the surrounding bone, leading to early implant failure. When inserted in a healthy jaw, on the other hand, dental implants can last 20 years or more with proper care.
2. Enhanced aesthetic outcomes.
By providing a more even surface on which to mount dental implants (and other restorations), bone grafting ensures superior aesthetic results and correct bite alignment. Bone grafting also promotes the growth of healthy, symmetrical gum tissue, which prevents visible gaps from forming between the implant crown and the gum line.
In addition to these benefits, bone grafting can correct issues with facial alignment that often arise after bone loss, such as a sunken facial appearance, loss of facial contours, and loose skin around the jawline. As such, eligible patients can achieve improved facial harmony and a more natural-looking smile through bone grafting.
3. Prevention of further bone loss.
Bone grafting helps prevent further bone resorption or shrinkage in areas where teeth have been lost or extracted. Without bone grafting, the jawbone may continue to deteriorate over time, leading to unwanted changes in facial appearance and limiting the patient’s options for smile restoration.
Potential Risks and Considerations
Bone grafting is a low-risk procedure, but any surgery carries a possibility of complications. Usually, issues after bone grafting are minor and preventable with correct post-surgical aftercare and routine follow-ups. Some potential complications of bone graft surgery include donor tissue rejection, infection, osseointegration failure, and the migration of donor tissue. Your risk of complications may be higher if you have periodontal disease or health conditions that could potentially interfere with healing.
To reduce your risk of experiencing complications, choose a dental implant surgeon with specific training and experience performing bone grafts. Then, verify that your surgeon uses the latest bone grafting techniques to help ensure a successful outcome. Over the last decade, emerging technologies, such as using platelet-rich plasma (PRP), platelet-rich fibrin (PRF), and plasma rich in growth factors (PRGF) to expedite bone regeneration, have significantly reduced the risk of complications following bone graft surgery. Growth factors have been shown to enhance the quality and strength of bone grafts, which is a significant aspect of preventing graft failure. Other promising advances in dental bone grafting include peptide therapy, cell-based therapy, genetic therapy, scaffolds, and medical lasers, which stimulate tissue regeneration.
Recovery and Aftercare
Because dental bone grafting is a minimally invasive surgical procedure, most patients feel better within a week or two of having surgery and have little or no swelling or discomfort. However, patients must remember that complete bone healing and osseointegration takes three to nine months. During this time, it is essential to practice correct aftercare to reduce the risk of complications. In addition to providing pain relief, your dentist will ask you to adhere to specific oral hygiene practices and dietary restrictions.
Though aftercare instructions may vary based on the type and complexity of the bone graft a patient receives, some general guidelines to keep in mind include:
– Plan for postoperative rest. In the first 48 hours after surgery, rest and avoid vigorous exercise and heavy lifting. Apply a cold compress to your cheek over the treatment area several times daily to reduce swelling
– Manage pain and prevent infection. Take pain medication as prescribed for the first ten days after your procedure. If you have also been prescribed antibiotics, be sure to complete the entire course. Monitor for signs of infection, such as redness and inflammation around the surgical site, new or worsening pain, fever, and fatigue, and contact your dentist immediately if you experience these symptoms.
– Adjust your oral hygiene routine. While it is essential to keep the surgical site clean to prevent infection, you should be gentle when brushing and flossing and avoid disturbing the area around the bone graft. Your dentist may provide specific instructions on how to clean your teeth and gums without disrupting the healing process. Do not rinse your mouth or spit out fluids for the first 24 hours after surgery to prevent dislodging the blood clot. After 24 hours, you may gently rinse your mouth with a sterile saline solution to clean the incision site.
– Eat soft foods: For at least two weeks after your bone grafting procedure, you will be asked to stick to a soft diet to avoid putting excessive pressure on the surgical site. Foods such as yogurt, smoothies, mashed potatoes, soups, and scrambled eggs are gentle on the healing area. Avoid hot, spicy, crunchy, or hard foods that may irritate the surgical site.
– Avoid tobacco and alcohol: Smoking and alcohol consumption can hinder the healing process and increase the risk of complications after dental bone grafting. Refrain from smoking and limit alcohol intake for at least a month following surgery to promote optimal healing.
– Protect the surgical site: Avoid touching or disturbing the surgical site with your tongue, fingers, or any foreign objects, such as drinking straws. If a protective barrier membrane was placed over the surgical site, don’t remove it without your dentist’s permission (most barriers are designed to dissolve naturally over time and do not require removal).
– Attend follow-up appointments: Be sure to attend all scheduled follow-up appointments with your dental care provider. These visits allow your dentist to monitor your healing progress, assess bone regeneration, and address any concerns or complications as soon as possible. Follow-up appointments are essential for ensuring the success of your bone grafting procedure.
Dr. Oscar Dalmao - Over 30 Years of Dental Implants and Dental Bone Graft Procedures
If you have missing teeth, getting dental implants is one of the best ways to improve oral health. Along with preventing jawbone deterioration, dental implants prevent bite misalignment by supporting your remaining teeth, ensuring they stay in position. Likewise, by preserving an even bite force, dental implants significantly reduce the risk of your other teeth becoming prematurely worn, chipped, cracked, loose, or broken. Many patients with missing teeth experience further dental deterioration due to these factors unless they have restorative treatments.
Though the idea of undergoing bone grafting may seem intimidating, it is crucial to keep these advantages in mind if your dentist indicates you are a good candidate for this procedure. By choosing a skilled, experienced oral surgeon, you can ensure a successful outcome and quick recovery while knowing your dental implants will last many years – giving you the freedom to eat, speak, and smile confidently.
As one of Mississauga’s leading oral surgeons and dental implant specialists, Dr. Oscar Dalmao can help you understand your dental restoration options and create a treatment plan that works for you. With guidance from our compassionate team of experts, you can achieve a healthy, functional smile after tooth loss.
For more information on dental implants and bone grafting, contact Dr. Dalmao and Associates today.
